The term “burnout” dates as far back as 1974. Coined by psychologist Herbert J. Freudenberger in a Journal of Social Issues article entitled “Staff Burnout,” he discussed job dissatisfaction precipitated by work-related stress.
Presently, burnout is included in the World Health Organization’s (WHO) 11th Revision of the International Classification of Diseases (ICD-11)—as an occupational phenomenon, however.
Burnout is not classified as a medical condition.
In the WHO’s chapter on factors influencing health status or contact with health services, the agency includes reasons for which people contact health services that are not classed as illnesses or health conditions.
And in its definition of burnout as a syndrome, the WHO identifies three key components that contribute to chronic stress associated with work:
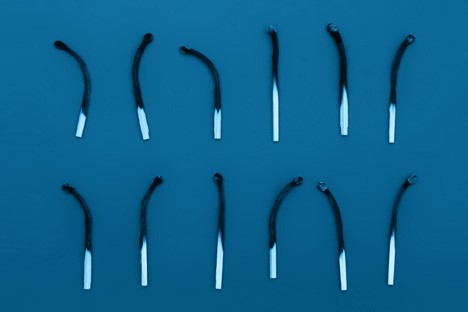
- Feelings of energy depletion or exhaustion;
- Depersonalization, feelings of cynicism, negativity;
- Reduced professional efficacy.
Burnout During Residency Training: A Literature Review
Distress during medical school and residency can lead to burnout—which, in turn, can result in negative consequences as a working physician. Prevalent in medical students (28%–45%), residents (27%–75%, though specialty dependent), and in practicing physicians (63%), burnout’s psychological distress and physical symptoms impact both work performance and patient safety. Specific contributors of said burnout include the following: time demands, lack of control, work planning and organization, as well as inherently difficult job situations and interpersonal relationships.
Fortunately, there are several workplace interventions for mentors to mitigate burnout with in-training physicians, such as wellness workshops, workload modifications (e.g., increased diversity of work duties), and better stress management education or appropriate emotional intelligence training.
As individuals, we have our own behavioral interventions to make: meditation, counseling, etc. Social interventions matter, too, especially when promoting our professional relationships. We can’t forget the importance of exercise and other physical activity either.
If not addressed, the risks of burnout are myriad. In addition to increased cardiovascular disease and inflammatory biomarkers, burnout elevates rates of depression and suicidal ideation. Thankfully, plans and attempts in burnout states do tend to decline with recovery.
Importantly, clinician depersonalization is associated with lower patient satisfaction and longer post discharge patient recovery time. So, we need to be able to identify elements of burnout—in ourselves and in others.
Physical symptoms:
- Insomnia
- Change in appetite
- Fatigue
- Colds or flu
- Headaches
- Gastrointestinal distress
Psychological symptoms:
- Low or irritable mood
- Cynicism
- Decreased concentration
- Can negatively affect productivity and rapport
Additional elements:
- Daydreaming
- Procrastination
- Increased alcohol or drug use
Recommended Reading:
The Moral Crisis of America’s Doctors | New York Times
Back from Burnout: Confronting the Post-Pandemic Physician Turnover Crisis (mgma.com)
Estimating the Attributable Cost of Physician Burnout in the United States – PubMed (nih.gov)
Physician Well-being 2.0: Where Are We and Where Are We Going? – Mayo Clinic Proceedings
Dr. Drosten’s ARRS “Sound of Wellness” Playlist Selection:
Delibes
Tchaikovsky
Mendelssohn
You may also be interested in
- ARRS Online Course: Sharpening Teamwork and Communication Skills
- AJR Live Webinar: Women’s Issues in IR, DR, and Professional Life
- ARRS Quick Bytes: Emergent Imaging: Improving CT Workflow and Image Quality