Khaled M. Elsayes
Professor of Diagnostic Radiology
University of Texas, MD Anderson Cancer Center and McGovern Medical School
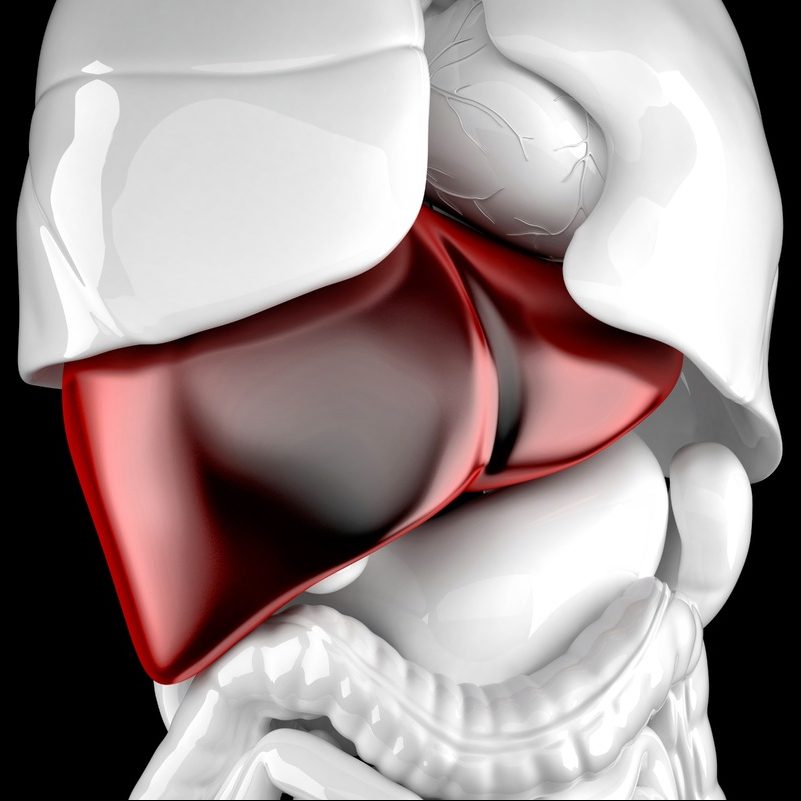
Chronic liver disease is an increasingly common and important disorder, now afflicting more than 25% of the world’s population. Regardless of its underlying cause, chronic liver disease can progress to cirrhosis, development of liver cancer, and liver-related death. Recent advances in imaging knowledge and technology have elevated the role of radiology in the diagnosis and management of patients with or at risk for chronic liver disease across its entire spectrum and course.
Noninvasive Monitoring of Chronic Liver Disease
With a rising epidemic of obesity and metabolic syndrome in the United States, nonalcoholic fatty liver disease and its progressive form, nonalcoholic steatohepatitis, are increasingly encountered in practice. Additionally, overconsumption of alcohol and viral hepatitis remain common causes of chronic liver disease. Irrespective of etiology, chronic liver disease represents a spectrum of inflammation, injury, fibrosis, and eventually, cirrhosis. Although in the past, cirrhosis was considered an irreversible injury, recent medical advances provide opportunities to halt and even reverse fibrosis. Likewise, identification and modulation of risk factors, like fat and iron deposition in the liver, are essential to managing patients at risk for or with chronic liver disease. Pathological assessment remains a reference standard, but risks and cost associated with biopsy reduce the benefit in the setting of longitudinal monitoring. Radiologists play an essential role in providing noninvasive quantitative information to direct management.
State of the art imaging options for assessing chronic liver disease focus on three key elements: liver fat, iron, and fibrosis. Liver fat can be identified by ultrasound, CT, and MRI. The most accurate, accessible, and precise method for monitoring patients with chronic liver disease is MRI-proton density fat fraction (PDFF). MRI-PDFF takes advantage of the fact that owing to differences in molecular structures, fat and water protons experience different magnetic fields and precess at different rates. This offset in frequency (“chemical shift”) is the basis for in- and opposed-phase dual echo imaging with its familiar appearance, including “India ink” etching at fat-water interfaces on opposed-phase images, due to signal cancellation when water and fat are precessing directly opposite each other. MRI-PDFF expands on this concept and is estimated by acquiring images at multiple echo times, selected to optimize separation of fat and water signals, and by taking into account several confounders that otherwise introduce errors into fat quantification. Iron is one of the most important confounders and is also an important factor contributing to chronic liver disease. Iron is ferromagnetic and causes signal decay (T2*), due to disruption of local magnetic fields. The decay of signal over time (R2*) is directly proportional to iron content over a wide pathophysiological spectrum, allowing us to estimate R2* values and convert them to liver iron concentrations. Hence, MRI-PDFF quantifies both fat and iron.
The most validated and clinically used method for estimating liver fibrosis is elastography. Elastography can be done with ultrasound or MRI. Elastography is an imaging technique that quantifies the stiffness of tissue, or resistance to deformation following application of external pressure. Imaging methods estimate stiffness by generating shear waves in the liver and measuring their propagation. Ultrasound methods differ based on how they generate shear waves and whether they produce gray-scale images (point shear wave elastography and 2D elastography) or not (vibration controlled transient elastography). Ultrasound methods measure shear wave speed, which can be converted into tissue stiffness values. The speed measurements may differ between manufacturers and etiologies of chronic liver disease, which challenges establishment of universal thresholds for stages of fibrosis. Magnetic resonance elastography (MRE) utilizes a standard system for shear wave generation and measurement across all vendors and platforms; as a result, the tissue stiffness values obtained from MRE are thought to be more reproducible.
Standardizing Diagnosis of Liver Cancer in Patients with Chronic Liver Disease
Hepatocellular carcinoma (HCC) can be confidently diagnosed based on imaging, in contradistinction to most malignancies that require tissue examination for their diagnosis. The noninvasive diagnosis of HCC is justified by the high positive predictive value of CT and MRI for this purpose when stringent criteria are applied in high-risk patients (i.e., high pre-test probability).
Current standards in the noninvasive diagnosis of HCC follow the guidelines of the American Association for the Study of Liver Disease (AASLD), Organ Procurement and Transplantation Network (OPTN), and Liver Imaging Reporting and Data System (LI-RADS).
Guo J, Seo Y, Ren S, et al. Diagnostic performance of contrast-enhanced multidetector computed tomography and gadoxetic acid disodium-enhanced magnetic resonance imaging in detecting hepatocellular carcinoma: direct comparison and a meta-analysis. Abdom Radiol (NY) 2016; 41:1960–1972
Liu X, Jiang H, Chen J, Zhou Y, Huang Z, Song B. Gadoxetic acid disodiumenhanced magnetic resonance imaging outperformed multidetector computed tomography in diagnosing small hepatocellular carcinoma: a meta-analysis. Liver Transpl 2017; 23:1505–1518
LI-RADS is a comprehensive system that provides standards for terminology, technique, interpretation, and reporting of liver imaging. It has been developed by a multi-disciplinary and increasingly international team of diagnostic and interventional radiologists, hepatobiliary surgeons, hepatologists, and hepatopatholgists, alongside support from the American College of Radiology.
Kim BR, Lee JM, Lee DH, et al. Diagnostic performance of gadoxetic acid-enhanced liver MR imaging versus multidetector CT in the detection of dysplastic nodules and early hepatocellular carcinoma. Radiology 2017; 285:134–146
Nakamura S, Nouso K, Kobayashi Y, et al. The diagnosis of hypovascular hepatic lesions showing hypo-intensity in the hepatobiliary phase of Gd-EOBDTPA-enhanced MR imaging in high-risk patients for hepatocellular carcinoma. Acta Med Okayama 2013; 67:239–244
LI-RADS assigns a diagnostic category code for each observation to communicate the likelihood of being benign or being HCC, ranging from LR-1 (definitely benign) to LR-5 (definitely HCC). The LR-5 category has a reported specificity of 95% for HCC. In addition to the previous five categories, LI-RADS also provides three other categories—LR-NC (not categorizable), LR-TIV (tumor in vein), and LR-M (probably or definitely malignant, not necessarily HCC)—with certain criteria for each category.
The imaging diagnosis of HCC in LI-RADS is based on the presence or absence of five major imaging features and a number of ancillary features (AFs). Major features include nonrim arterial phase hyperenhancement (APHE), nonperipheral “washout” appearance, enhancing “capsule” appearance, size, and threshold growth.
The AFs are divided into three groups: AFs that favor malignancy in general, AFs that favor HCC in particular, and AFs that favor benignity. A preliminary LI-RADS category is assigned based on the present major features, then the AFs are used at the interpreter’s discretion to adjust the preliminary category.
In summary, the latest advances in imaging of HCC allow for a confident noninvasive diagnosis of this malignancy and comprehensive assessment of other lesions and pseudolesions depicted by imaging.
Improving Sensitivity for Liver Cancer Diagnosis with HBAs
HBAs are gadolinium-based intravenous MR contrast agents that permit hepatobiliary phase (HBP) imaging, in addition to conventional dynamic post-contrast phases. Gadoxetate disodium is the most commonly utilized HBA, due to high hepatobiliary excretion and convenient HBP timing of 10–30 minutes.
Gadoxetate offers several advantages for patients with cirrhosis. Of all available modalities, gadoxetate-enhanced MRI has the highest overall per-lesion sensitivity (86%) and positive predictive value (94%) for diagnosis of HCC, as well as the highest sensitivity (84–96%) for detection of ≤ 2 cm HCCs. Unlike APHE, reduced gadoxetate uptake is an early event in hepatocarcinogenesis: up to 38% of early HCCs may be seen only on the HBP, and 82% of high-grade dysplastic nodules (DN) and 76% of early HCCs are hypointense on the HBP.
HBP hypointense nodules without APHE are unique to HBA MRI. If sampled histologically, 74% of such nodules are HCCs, and 10% are DN, although these numbers may be inflated by selection bias; if followed, 16–43% progress to hypervascular HCC within 24 months.
Cho YK, Kim JW, Kim MY, Cho HJ. Non-hypervascular hypointense nodules on hepatocyte phase gadoxetic acid-enhanced MR images: transformation of MR hepatobiliary hypointense nodules into hypervascular hepatocellular carcinomas. Gut and Liver 2018; 12:79–85
Saitoh T, Sato S, Yazaki T, et al. Progression of hepatic hypovascular nodules with hypointensity in the hepatobiliary phase of Gd-EOB-DTPA-enhanced MRI in hepatocellular carcinoma cases. Intern Med 2018; 57:165–171
Yang HJ, Song JS, Choi EJ, Choi H, Yang JD, Moon WS. Hypovascular hypointense nodules in hepatobiliary phase without T2 hyperintensity: longterm outcomes and added value of DWI in predicting hypervascular transformation. Clin Imaging 2018; 50:123–129
Hwang JA, Kang TW, Kim YK, et al. Association between non-hypervascular hypointense nodules on gadoxetic acid-enhanced MRI and liver stiffness or hepatocellular carcinoma. Eur J Radiol 2017; 95:362–369
Briani C, Di Pietropaolo M, Marignani M, et al. Non-hypervascular hypointense nodules at gadoxetic acid MRI: hepatocellular carcinoma risk assessment with emphasis on the role of diffusion-weighted imaging. J Gastrointest Cancer 2018; 49:302–310
Kim YS, Song JS, Lee HK, Han YM. Hypovascular hypointense nodules on hepatobiliary phase without T2 hyperintensity on gadoxetic acid-enhanced MR images in patients with chronic liver disease: long-term outcomes and risk factors for hypervascular transformation. Eur Radiol 2016; 26:3728–3736
Rosenkrantz AB, Pinnamaneni N, Kierans AS, Ream JM. Hypovascular hepatic nodules at gadoxetic acid-enhanced MRI: whole-lesion hepatobiliary phase histogram metrics for prediction of progression to arterial-enhancing hepatocellular carcinoma. Abdom Radiol (NY) 2016; 41:63–70
HBP hypointense nodules without APHE are also markers of increased HCC risk elsewhere in the liver: the cumulative three year rate of HCC elsewhere in the liver is 22%, compared to 6% in patients with no such nodules.
Lee DH, Lee JM, Lee JY, et al. Non-hypervascular hepatobiliary phase hypointense nodules on gadoxetic acid-enhanced MRI: risk of HCC recurrence after radiofrequency ablation. J Hepatol 2015; 62:1122–1130
Song KD, Rhim H, Lee MW, Kim YS, Kang TW. Intrahepatic distant recurrence after radiofrequency ablation for hepatocellular carcinoma: precursor nodules on pre-procedural gadoxetic acid-enhanced liver magnetic resonance imaging. Acta Radiol 2017; 58:778–785
The degree of gadoxetate uptake may predict tumor differentiation: poorly-differentiated HCCs are more frequently HBP hypointense (98%), compared with well- or moderately-differentiated HCCs (86%).
Kitao A, Matsui O, Yoneda N, et al. Hypervascular hepatocellular carcinoma: correlation between biologic features and signal intensity on gadoxetic acid-enhanced MR images. Radiology 2012; 265:780–789
Kitao A, Zen Y, Matsui O, et al. Hepatocellular carcinoma: signal intensity at gadoxetic acid-enhanced MR Imaging–correlation with molecular transporters and histopathologic features. Radiology 2010; 256:817–826
Use of gadoxetate in patients with cirrhosis is associated with several important pitfalls. Smaller contrast dose and volume affect timing of the arterial phase (AP) and may lead to reduced peak enhancement of HCC in the AP.
Tirkes T, Mehta P, Aisen AM, Lall C, Akisik F. Comparison of dynamic phase enhancement of hepatocellular carcinoma using gadoxetate disodium vs gadobenate dimeglumine. J Comput Assist Tomogr 2015; 39:479–482
Davenport MS, Bashir MR, Pietryga JA, Weber JT, Khalatbari S, Hussain HK. Dose-toxicity relationship of gadoxetate disodium and transient severe respiratory motion artifact. AJR 2014; 203:796–802
Kim SY, Park SH, Wu EH, et al. Transient respiratory motion artifact during arterial phase MRI with gadoxetate disodium: risk factor analyses. AJR 2015; 204:1220–1227
Portal venous phase (PVP) “washout” appearance in combination with APHE allows for nearly 100% specificity of HCC diagnosis.
In patients with decompensated cirrhosis, diminished parenchymal uptake of gadoxetate results in less enhancement during the TP and the HBP.
Although HBP hypointensity improves detection of HCC and high-grade DN, TP and HBP hypointensity are not specific to HCC, as any lesion without functional hepatocytes (e.g., cysts, hemangiomas, non-HCC malignancies, etc.) will appear hypointense in the HBP.
In conclusion, use of gadoxetate in patients with cirrhosis offers certain advantages—particularly higher sensitivity for HCC, if liver function is preserved and AP quality is adequate—but radiologists should be aware of the various pitfalls of gadoxetate to optimize patient selection and image interpretation.
Acknowledgements
Kathryn Fowler, Claude Sirlin, and Victoria Chernyak also contributed to this article.
The opinions expressed in InPractice magazine are those of the author(s); they do not necessarily reflect the viewpoint or position of the editors, reviewers, or publisher.