Reiterating, the house of radiology’s influence in shaping our nation’s health care policy writ large, the American Medical Association (AMA) House of Delegates (HOD) advanced several measures with significant implications for American Roentgen Ray Society (ARRS) members during its own annual meeting in Chicago this June.
In short: expect DICOM mandates to simplify imaging transfers, elevated oversight of AI, and more rigorous validation for CT-based calcium scoring [1].
Finally, Federally Interoperable DICOM
The HOD passed a pivotal resolution calling on AMA advocacy for federal health IT interoperability standards to include the DICOM format, a critical “missing link” that delegates have long championed. Despite over two decades of EHR development and federal mandates, DICOM has been excluded from formal interoperability frameworks. As a result, radiological images frequently cannot travel seamlessly through EHR systems, frustrating patients and providers alike. For one example, patients arriving for mammograms at new facilities are often dumbfounded that previous studies cannot be accessed digitally from elsewhere. The absence of interoperable imaging standards contributes to delayed care, redundant exams, unnecessary radiation exposure, and burdens for patients. And the security risks are legion (Fig. 1).
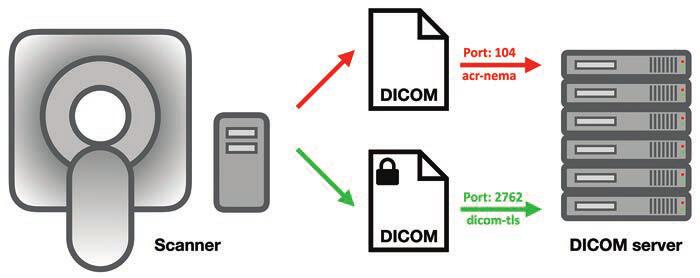
Fig. 1—Schematic shows DICOM server, computers that can exchange and store DICOM objects. Server offers DICOM service, which is software that can send and receive DICOM messages, running via specific computer ports (i.e., communications channels). Secured DICOM service is known as dicom-tls (port 2762), which uses transport layer security for negotiations, authentication, and encryption. A service that cannot be queried by hackers because it uses strong authentication mechanisms, this service sends and receives encrypted DICOM messages that cannot be read by hackers either. However, this is only true for manufacturers that have chosen to implement its strong authentication and encryption features. Arrows show direction of data transmission.
Spearheaded by neurology and orthopedic associations, this resolution urges inclusion of DICOM in the U.S. Core Data for Interoperability (USCDI) and seeks regulatory action requiring EHR and imaging archive vendors to support secure, efficient exchange of DICOM data. Testimony also highlighted policy fissures stemming from the Health Information Technology for Economic and Clinical Health (HITECH) Act of 2009, which exempted radiologists—alas, not viewed as patient-facing—from certain data-sharing requirements, thereby keeping imaging outside USCDI [2]. A significant win for medical imagers across the country, delegates did have to amend the resolution to get it passed, but this is meaningful progress toward closing the interoperability gap that hampers timely, coordinated, and secure care.
More Oversight and Transparency for AI
With AI digging even deeper into the specialty—at last count, over 75% of the more than 1,000 algorithms cleared by the Food and Drug Administration target radiology [3]—the HOD continued sounding the alarm on the “black box” nature of so many machine-learning, deep-learning, and radiomic systems. Resolution 519, though not adopted thanks to too much overlap with AMA’s existing AI policies, successfully highlighted acute issues of explainability, advocating for evidence-based, transparent AI within a deliberately structured framework [4]. Aligning with AMA’s stance that the physician’s expertise remains central to clinical decision-making, everyone in Chicago agreed that today’s radiologists must be able to comprehend and articulate how generative AI, agentic AI, or some future proprietary amalgam of the two arrives at any given verdict. All too often, seemingly slight updates to vendor hardware, scanning protocol, or patient demographics end up altering algorithmic performance, further underscoring the need for responsible vetting and robust monitoring of AI.
No LDCT for Coronary Calcium, Yet
AMA also tabled a resolution regarding expanded promotion and usage of low-dose CT (LDCT) to screen both lung cancer and coronary artery disease via coronary calcium scoring. Emphasizing the modality’s value as a public health tool for high-risk individuals, particularly those with pack-year history of smoking, LDCT delivers far less radiation than standard CT and can detect small lung nodules early. Indeed, crucial research from the National Lung Screening Trial shows it can reduce lung cancer mortality by up to 20% [5].
And yet, uptake is still cripplingly low; fewer than 6% of eligible patients receive LDCT screening. To buttress the resolution’s goals, the American College of Radiology is launching complementary efforts, including expanding its early lung cancer registry to capture incidental findings from routine CTs, not just formal screening exams [6]. Such distinction will deepen insights into nodule detection and follow-up.
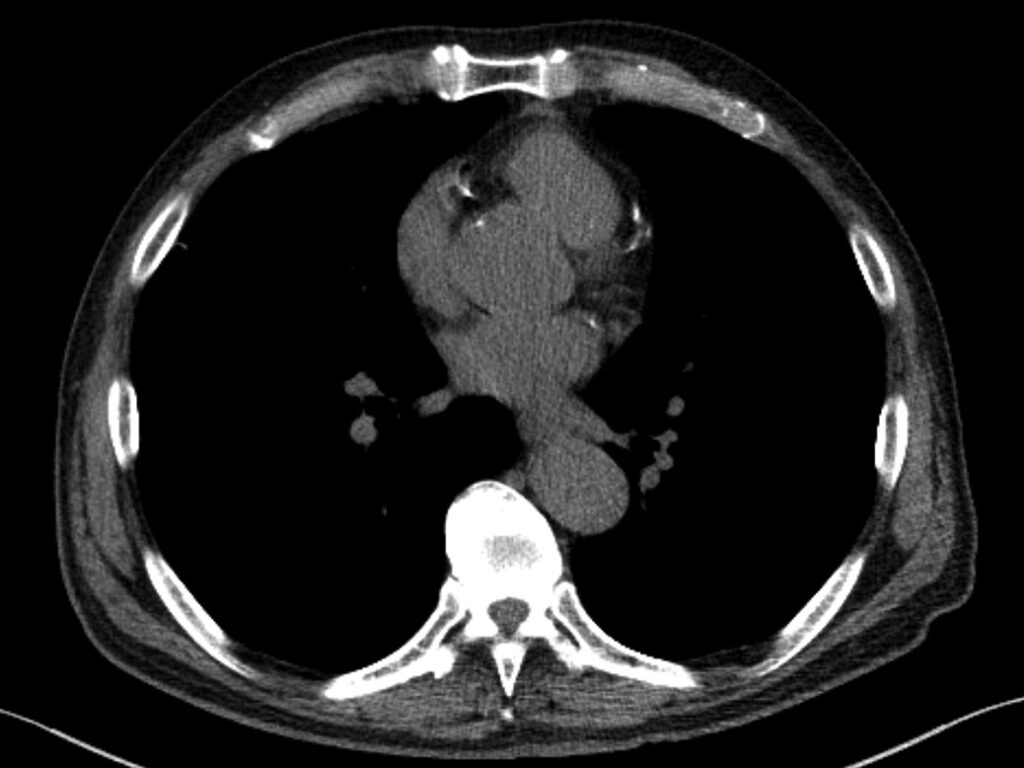
Fig. 2—73-year-old patient who underwent lung cancer screening by LDCT of the chest. Axial CT image shows coronary artery calcification (CAC). CAC was assessed as severe by consensus visual analysis.
More broadly, many hospitals have begun offering low- or no-cost LDCT screenings as an entry point for preventive care. Apropos, this resolution specifically solicits a coordinated national effort of public awareness campaigns and provider education to ensure affordable, widespread access to this potentially life-saving tool.
For further details about the 2025 Annual Meeting of the HOD, click here.
References:
- ACR highlights key AMA meeting measures. Aunt Minnie website. www.auntminnie.com/practice-management/associations/news/15749013/acr-highlights-key-ama-meeting-measures. Published June 20, 2025. Accessed August 13, 2025
- Fornell D. Radiologists call on AMA to push for new federal IT interoperability standards. Radiology Business website. radiologybusiness.com/topics/medical-imaging/radiologists-call-ama-push-new-federal-it-interoperability-standards. Published June 24, 2025. Accessed August 13, 2025
- Carey L. Radiology drives July FDA AI-enabled medical device update. Aunt Minnie website. www.auntminnie.com/imaging-informatics/artificial-intelligence/article/15750598/radiology-drives-july-fda-aienabled-medical-device-update. Published July 14, 2025. Accessed August 13, 2025
- Specialty and Service Society (SSS) 2025 Annual Meeting of the House of Delegates. AMA website. www.ama-assn.org/system/files/a25-sss-agenda-resolution-grid.pdf. Accessed August 13, 2025
- National Lung Screening Trial. NIH National Cancer Institute website. www.cancer.gov/types/lung/research/nlst. Accessed August 13, 2025
- Fornell D. AMA resolution backs expanded low-dose CT screenings for lung cancer, heart risk. Radiology Business website. radiologybusiness.com/topics/medical-imaging/computed-tomography-ct/ama-resolution-backs-expanded-low-dose-ct-screenings-lung-cancer-heart-risk. Published June 20, 2025. Accessed August 13, 2025
