Dual-energy CT (DECT) has become a workhorse in emergency imaging, particularly for iodine mapping and virtual noncontrast applications. But as Aaron Sodickson, MD, reveals in a presentation now available in the ARRS Quick Bytes library, conventional DECT systems come with a quiet limitation: dual-energy information is not uniformly available across the entire field of view. Photon-counting CT (PCCT) changes that.
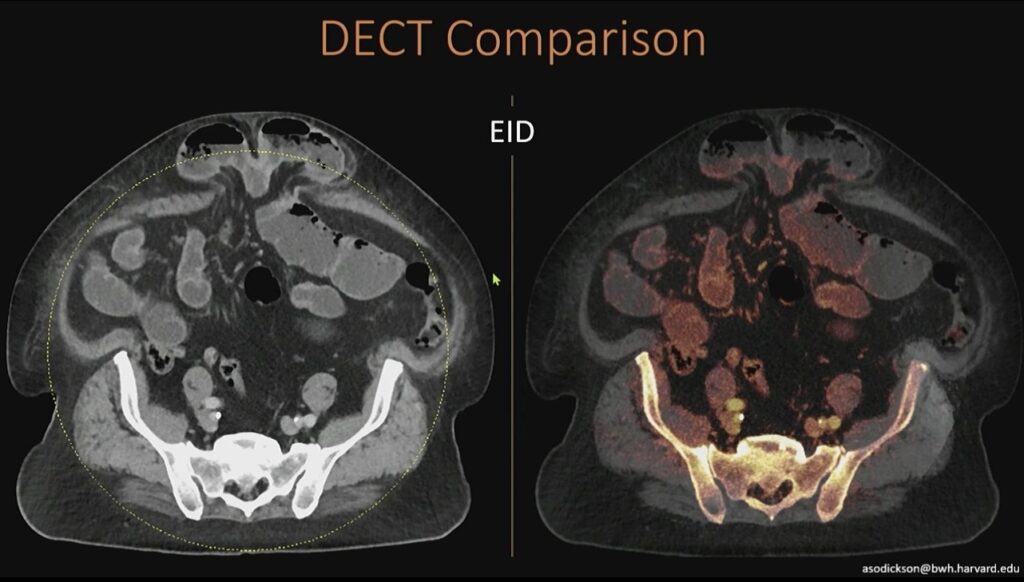
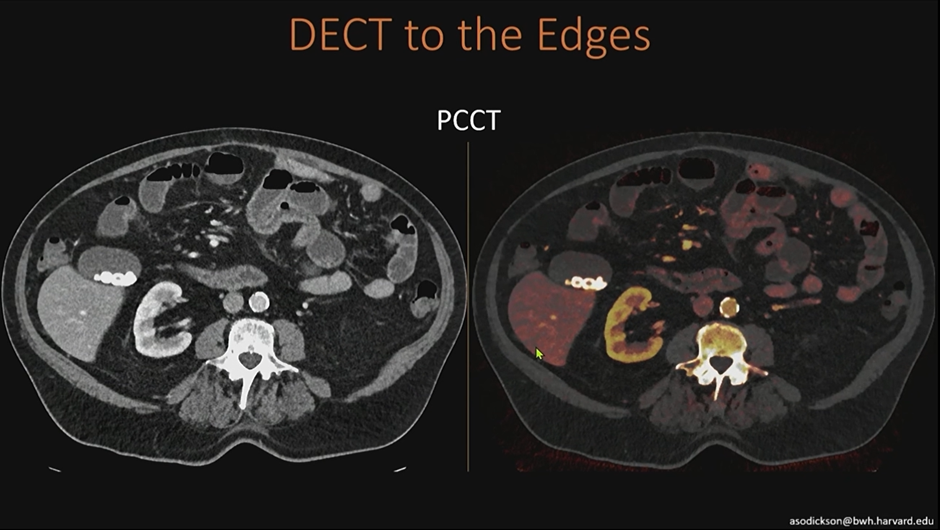
Conventional DECT’s Limitations: On many high-end dual-energy scanners, iodine maps are only reliable within a central circular region. Outside that area, dual-energy information is lost. In large patients or peripheral anatomy, this can mean incomplete iodine characterization and diagnostic uncertainty.
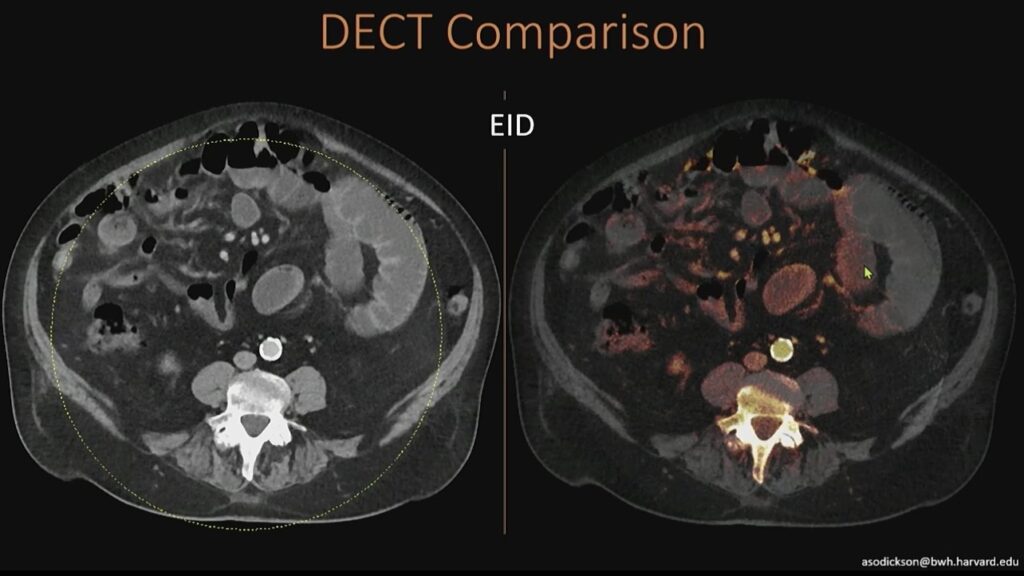
In practice, you may see clean iodine signal centrally, but nothing at the edges—simply because the system cannot acquire dual-energy data beyond that geometric constraint.
What Does PCCT Do Differently? PCCT acquires spectral information directly at the detector. Because it does not rely on paired detector geometries or source-based separation, dual-energy information is available across the entire field of view, meaning:
- Iodine maps extend fully to the periphery
- Large patients no longer “fall outside” the dual-energy zone
- Edge anatomy benefits from the same spectral data as the center
In the ED, where patient size and positioning are unpredictable, this matters.
Improved Noise Behavior in Iodine Maps: Another practical advantage of PCCT is cleaner iodine post-processing. On conventional DECT, iodine maps may show speckled signal in non-enhancing structures—algorithmic noise that can mimic low-level enhancement.
In this example below of a renal cyst, conventional DECT shows scattered orange signal that is not true enhancement. On PCCT, that noise is substantially reduced, allowing confident classification of a benign, non-enhancing complex cyst.
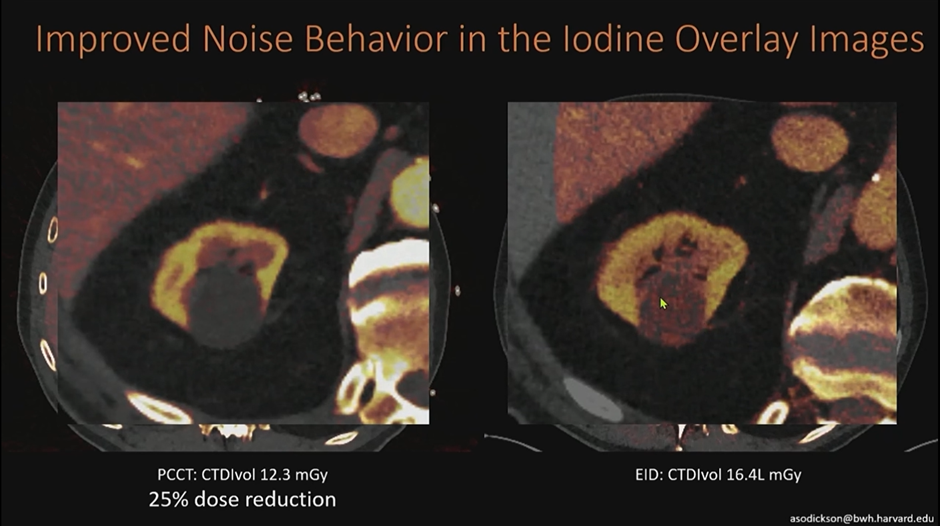
There isn’t actually enhancement within this cyst; this is noise in the algorithm. On the photon-counting scanner, we’re able to knock down that noise to see much more cleanly that this is a non-enhancing, benign, complex cyst.
Why This Matters in the ED: ED radiology rewards speed and certainty. PCCT improves both by:
- Preserving iodine data across the entire image
- Reducing false-positive enhancement
- Increasing confidence in lesion characterization
- Decreasing the need for follow-up imaging
Bottom Line: Photon-counting CT removes the “edge problem” of conventional DECT. By delivering full-field spectral data with improved noise characteristics, PCCT strengthens iodine-based interpretation—exactly where ED imaging needs it most.

Leave a Reply