Eric Dietsche, MD
Department of Diagnostic Imaging, Rhode Island Hospital
Warren Alpert Medical School, Brown University
John Scaringi, MD
Department of Diagnostic Imaging, Rhode Island Hospital
Warren Alpert Medical School, Brown University
First question: should radiologists really be performing inpatient fludeoxyglucose (FDG) PET/CT? Our recent nuclear medicine editorial in the American Journal of Roentgenology (AJR), “Inpatient FDG PET/CT: Counterpoint—A Costly Yet Subpar Evaluation That Prolongs Hospital Length of Stay,” highlights key problems with this diagnostic pathway [1], as well as why it may be preferably to defer inpatient PET examinations in most clinical scenarios.
No doubt, the volume of imaging studies is increasing nationwide. According to ARRS’ own estimates [2], U.S. radiologists perform some 80 million CTs each year—probably more. Those are just the examinations we are able to track via billing data.
PET/CT is no exception to rising volumes. In fact, one Journal of Nuclear Medicine single-center study reported a greater than five times increase in inpatient PET/CT examinations over a 10-year period at the authors’ institution [3]. Despite the increasing utilization of inpatient PET/CT, the procedure, itself, can be limited by both questionable clinical rationale and poor study quality. Moreover, due to distinct differences in reimbursement between inpatient and outpatient PET procedures, your health care system will likely get paid less for performing inpatient studies.
Quite often, the quality of PET/CT is limited in inpatient settings. Contributing factors to this suboptimal image quality include higher mean blood glucose levels. Patient motion remains a factor, too. As noted in Annals of Nuclear Medicine, acute processes (e.g., infection) also continue to confound our interpretations [4].
So, another question: what do all three of these FDG PET/CT studies here (Fig. 1) have in common that could be contributing to their poor image quality?
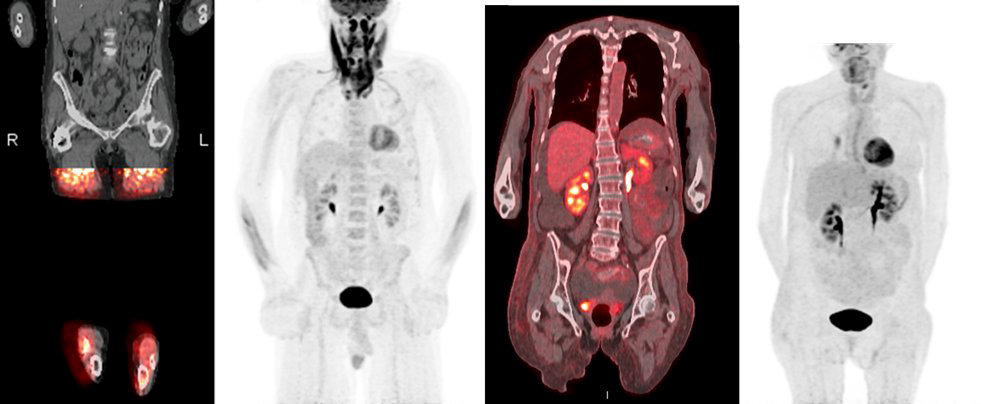
Fig. 1—First patient could not tolerate examination. Second patient suffering from respiratory distress. Third patient receiving course of high-dose steroids, resulting in altered biodistribution of fludeoxyglucose F18.
PET/CT is often ordered on an inpatient basis for initial oncologic staging. However, if there is no plan to initiate treatment while admitted to the hospital, an inpatient PET may only result in a substandard examination, while not changing patient management.
Given that PET/CT examinations are regularly booked weeks in advance, scheduling an inpatient study is challenging, frequently requiring a cancellation in the outpatient setting. This disruption can lead to prolonged patient stays, which increase overall costs and the risk of health care-associated adverse events.
Speaking of cost, inpatient PET/CT is costly to the health care system. Private insurance may not cover an inpatient PET, since the examination is typically viewed as an outpatient study. It is also worth noting that the Centers for Medicare & Medicaid Services bundle inpatient costs—with hospitals possibly receiving reduced or even no payment for high-cost items (i.e., PET/CT).
To reiterate our points, PET/CT in the inpatient setting is a pricey, subpar test that can potentially provide misleading diagnostic information to referring clinicians and patients. With rare exceptions, radiologists should counsel referring providers to skip the inpatient PET…and order an outpatient study instead.
Not everyone agrees with us, of course. For the opposing perspective, we urge you to cross-reference the original AJR Point, “A Strategic Path to Patient-Centered Yet Cost-Effective Care,” by two diagnostic radiologists from Oregon Health & Science University in Portland: Laszlo Szidonya, MD, PhD, and Nadine Mallak, MD [5].
References
- Dietsche E, Scaringi J. Inpatient FDG PET/CT: Counterpoint—A Costly Yet Subpar Evaluation That Prolongs Hospital Length of Stay. AJR 2024. Jul; 223:e2330655. doi: 10.2214/AJR.23.30655
- Munden RF. Disruptors of the Radiology Workforce—The Next Generation. ARRS InPractice website. www.radfyi.org/2024-arrs-in-training-issue. Published August 12, 2024. Accessed August 16, 2024.
- Crandall J, Gajwani P, Wahl R. Trends in Utilization of FDG PET/CT in an Inpatient Population. J Nucl Med 2016. May; 57(suppl 2):1771
- Yan X, Kang J, Zhou Y, et al. Imaging Quality of F-18-FDG PET/CT in the Inpatient Versus Outpatient Setting. Ann Nucl Med 2013. Jul; 27:508-14. doi: 10.1007/s12149-013-0714-8
- Szidonya L, Mallak N. Inpatient FDG PET/CT: Point-A Strategic Path to Patient-Centered Yet Cost-Effective Care. AJR 2024 Jul; 223:e2330585. doi: 10.2214/AJR.23.30585